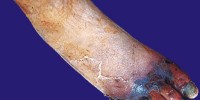
Diabetic ulcer
Condition, Causes and Symptoms
Diabetic foot ulcer is a major complication of diabetes mellitus, and probably the major component of the diabetic foot.
A skin ulcer is where an area of skin has broken down and you can see the underlying tissue. Most skin ulcers occur on the lower legs or feet. The skin normally heals quickly if it is cut. However, in some people with diabetes the skin on the feet does not heal so well and is prone to developing an ulcer. This can be even after a mild injury such as stepping on a small stone when you are bare feet.
Ulcers form due to a combination of factors, such as lack of feeling in the foot, poor circulation, foot deformities, irritation (such as friction or pressure), and trauma, as well as duration of diabetes.
Blisters and sores appear on numb areas of the feet and legs such as forefoot, heel region and as a result of numbness, pressure or injury that goes unnoticed and eventually become portal of entry for bacteria and infection.
In addition, having diabetes means you are more likely to have infections and an infection in the ulcer can occur. Occasionally, more serious problems can develop, such as gangrene.
Vascular disease can complicate a foot ulcer, reducing the body’s ability to heal and increasing the risk for an infection.
Elevations in blood glucose can reduce the body’s ability to fight off a potential infection and also retard healing.
- 15% percent of all diabetics will develop chronic wounds.
- Diabetic patients have a 15-fold increase of amputation risk.
- Major increase in mortality among diabetic patients, observed over the past 20 years is considered to be due to the development of vascular complications, including failure of the wound healing process.
- Diabetes-related amputations could be reduced by 50 percent if patients are routinely tested for neuropathy, educated to prevent complications and fitted with appropriate footwear.
Neuropathy, or nerve damage, is one of the most common complications of diabetes. Neuropathy develops gradually, usually in the feet, and results in numbness. This is a warning sign of diabetes. If you have numbness in your toes or feet, be sure to tell your doctor.
Diabetic ulcers are the most common cause of lower extremity amputation. 85 % of all amputations are preceded by a foot ulcer. To prevent amputation, it is important to diagnose and treat the ulcer as early as possible. One of the most important factors relating to the outcome of a diabetic foot ulcer is peripheral arterial disease (PAD).
- Test that you have a good blood circulation to the area. This is called an ankle brachial index.
If the ankle brachial index is 0.9 or less, you should see a vascular surgeon and/or interventional cardiologist to determine if intervention is necessary. “An ankle brachial index of 0.9 or below could point to a 50% occlusion of a major artery.”
This means putting it in a special custom-designed support footwear — such as the Air Walker or Off-loading Sandals. “This may be bulky, but it’s absolutely necessary until you heal”
Treatment
The primary goal in the treatment of foot ulcers is to obtain healing as soon as possible. The faster the healing, the less chance for an infection.
Not all ulcers are infected; however if your podiatric surgeon diagnoses an infection, a treatment program of antibiotics, wound care, and possibly hospitalization will be necessary.
Foot ulcers in diabetes require multidisciplinary assessment, usually by diabetes specialists and surgeons. Treatment consists of appropriate dressings, culture specific antibiotics, debridement, arterial revascularisation and platelet-rich fibrin therapies.
The science of wound care has advanced significantly over the past ten years. The old thought of “let the air get at it” (keeping wound open) is now known to be harmful to healing.
We know that wounds and ulcers heal faster, with a lower risk of infection, if they are kept covered and moist

Prevention
The best way to treat a diabetic foot ulcer is to prevent its development in the first place. Recommended guidelines include seeing a foot care specialist on a regular basis i.e. at least once a year to evaluate if you are at high risk for developing a foot ulcer and implement strategies for prevention.
You are at high risk if you:
- Have high plantar pressure areas
- Have neuropathy,
- Have poor circulation,
- Have a foot deformity (i.e. bunion, hammer toe), which put pressure on points on the feet.
- Have feet prone to minor cuts, grazes, corns
- Have callosities, cuts, bruises, cracks, blisters, redness,
- Wear inappropriate or ill-fitting shoes, which can put pressure on your feet.
- Have leg problems which affect the way that you walk, or prevent you from bending to care for your feet.
- Have had a foot ulcer in the past.
- Have uncontrolled blood sugar. ,
- Have a high cholesterol level, high blood pressure or are overweight
- Have other complications of diabetes, such as kidney or eye problems.
- Smoking and alcohol habits,
- Have sedentary life style
Learning how to check your feet is crucial in noticing a potential problem as early as possible.
Inspect your feet every day—especially between the toes and the sole—for cuts, bruises, cracks, blisters, redness, ulcers, and any sign of abnormality.
Any problems that are discovered should be reported to your doctor as soon as possible, no matter how “simple” it may seem to you.
The key to successful wound healing is following “gold standard” of care:
- Regular foot examination and care by foot care specialist
- lowering blood sugar
- appropriate debridement of wounds
- treating any infection
- reducing friction and pressure
- proper wound off-loading
- restoring adequate blood flow
In many cases, foot ulceration can be prevented with appropriate healthcare, patient education and counselling. All patients with diabetes should have regular foot and footwear inspections.
The old saying, “an ounce of prevention is worth a pound of cure” was never as true as it is when preventing a diabetic foot ulcer.